Today’s translation from medspeak to English: Inflammatory white blood cells and inflammatory nerve cells, in relation to CRPS.
Elevated blood levels of inflammatory monocytes (CD14+ CD16+ ) in patients with complex regional pain syndrome
Here’s what the jargon means.
// ed. note: my comments and clarifications are picked out by those two slashes and the contraction for “editorial notation.”
One important factor in CRPS is inflammation that starts in the nerves. Microglia and astrocytes, which are the inflammatory and immune cells of the nervous system, get active enough to cause worse pain by themselves.
That’s a sparking astrocyte. Pretty, eh?
// ed. note: The inflammatory and immune responses are mixed blessings throughout the body. An immune response is uncomfortable; think about the last time you had the flu — sucked, huh? An inflammatory response can cause pain due solely to the inflammation, like with some kinds of arthritis. So, for the microglia and astrocytes to make pain worse is not a surprise, since that’s what immune response and inflammation can do anywhere.
One type of immune cells normally floating in your blood, called monocytes, can get into the brain and spinal cord and turn themselves into the nervous system’s immune cells, microglia. The added level of inflammatory/immune response leads to more pain.
// ed. note: Again, not as strange as it sounds. The body’s living cells all contain complete DNA, and they are designed to be both helpful and appropriate; heart cells transplanted into muscles become muscle cells, and muscle cells transplanted in the heart become very much like heart cells. So, for this type of small white blood cells to turn into microglia is reasonable.
These are microglia in various active states.
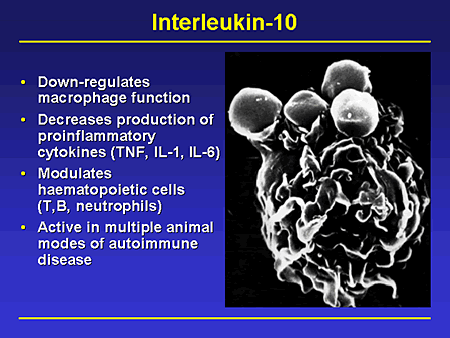
// ed. note: The inflammatory response releases cytokines. Cytokines are the chemical widgets, produced in inflammation, that serve as the chemical messengers running around the cells screaming that the sky is falling. Some cytokines increase inflammatory pain, some cytokines reduce it.
This study looked for particular kinds of inflammatory monocytes in the blood, to test the assumption that higher levels of these particular types of monocytes (which can then turn into microglia, making the inflammation and pain worse, etc.) are related specifically to CRPS.
Now here’s the fun part. The basic blood-borne indicators of inflammation and illness were no different in those with CRPS than in normal people. That’s why conventional lab results, like “complete” blood counts, come back normal for us. However, the proportion of the particular types of monocytes associated with CRPS, were significantly higher in those with CRPS. The type of cytokine that reduces inflammatory pain, was also significantly lower in people with CRPS.
That means the inflammatory process screws us coming and going, and screws specifically us, the people with CRPS, in ways that can be checked in a lab.
OK, GTK.
These are sensible scientists: they state that they don’t know if the monocyte proportions changed before or after the onset of CRPS, or both before and after. If before, it might indicate a predisposition to CRPS, in which case surgeries and accidents have to be handled with specific care for antioxidant therapy and aggressive pain control. If after, it might be relevant in figuring out how things are going and if what the doc is doing works.
Also, some drug company could make a staggering fortune off of new meds that mess with this process. They actually mention that at the end of the article, which means someone has to fund their work.
// ed. note: Be fair. We have a profit-based health care system driven by enormous corporations that are traded on the stock exchange, and the Sarbanes-Oxley laws mean that their first obligation is to their shareholders. Not patients. Not customers. But shareholders.
Conventional medicine has to come back to profitability. There are more direct ways to address these immune and inflammatory issues by existing means, which could be further developed, but they don’t sustain the pharma industry’s usual annual returns of 20-40% — a rate of stock profitability matched only by oil companies.
… On your pain.
If you have something to say about that, you can contact your political representatives here: http://www.usa.gov/Contact/Elected.shtml